Endoscopic Disc Decompression
Treatment for Slipped Disc, Herniated Disc, Nerve Impingement
Introduction
Bulging, protruding or herniated discs can result in immense pain and suffering for individuals with chronic back pain or nerve impingement. New developments in pain management techniques, such as minimal invasive spine surgery, have enabled our pain specialists to help many of such patients.
How did this happen?
A herniated lumbar intervertebral disc that has “slipped out” is actually a result of its gelatinous interior pushing its way through the outer wall can create a bulge or a protrusion that could cause pain, numbness or weakness due to spinal nerve impingement. Muscle weakness, sharp “shooting” pain or sensations, such as “pins and needles” often radiate from “pinched or compressed” spinal nerve root to the lower extremities.
Furthermore, when the spine degenerates because of aging, trauma or disease, the degenerated spine can also result in a disc pressing against a nerve root which makes it hard for the person to walk their usual distances, or do basic activities such as sitting or standing. Bending or flexing the back close to the injured disc usually causes a greater amount of pain.
What is Endoscopic Disc Decompression?
Endoscopic techniques for diagnostic purposes have been in use since the late 1970s. The endoscopic surgery techniques that became widely used in the 1990s for other surgical disciplines are now available for the interventional pain treatment of slipped disc and related spine conditions.
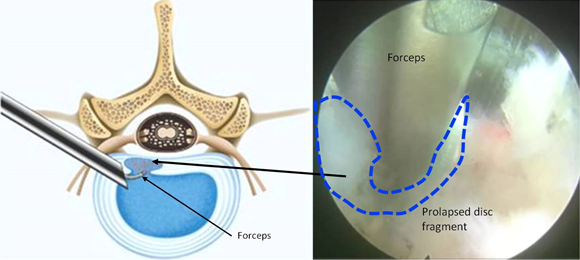
An endoscope is a long, hollow tube through which the specialist doctor can manipulate tiny instruments under direct visualisation. Normally, the tube is about 6-9 mm in diameter. Once the location of the protruding disk is identified, an instrument is inserted through the tube. It is used to take out tiny amounts of tissue from within the disc. This reduction in the disc’s interior volume allows the protrusion to recede, returning the disc to its original shape. This relieves the pressure from nearby nerve roots from herniated or bulging discs, and eases spinal canal pressure in the case of central disc protrusions. The procedure can be completed in under 60 minutes, after which a short recovery period and one follow-up appointment with the doctor is what you have left to do.
What are the advantages of a minimally invasive approach?
The best part of a minimally invasive spine surgery versus traditional, open spinal surgery is the lack of collateral damage to muscles, nerves and skin tissue. This method enables for quicker healing and recovery. Patients are usually surprised by the quick results they experience from this day procedure, though most will take about 1 week to get better.
Who is suitable for Endoscopic Disc Decompression?
If the symptoms can be alleviated through non-surgical means, surgery should not be necessary. We advise patients to consider traditional treatment methods first. However, if symptoms persist or even worsen, you might want to consider the least invasive procedure possible.
Debilitating chronic pain relief
After an endoscopic disc decompression, you will need to refrain from activities that might strain the affected area, such as lifting, for at least 2 weeks. However, most people can continue with their everyday lives after a week or two, as long as activities are limited to less strenuous work. Any discomfort that might occur as a result of the procedure is often significantly milder than debilitating chronic pain.
Seeking treatment for herniated disc or slipped disc? Contact us today.